Our bodies need different amounts of nutrients at each stage of life for growth, maintenance and repair. Older adults experience changes due to aging that present risks for malnutrition. These changes can lead to fatigue, memory loss, fractures, frailty and other health problems.
This guide discusses:
- Nutrients of concern for adults who are 60 and older.
- The bodily changes and physical limitations that can affect the nutritional status of older adults.
- Strategies that can help reduce risks for nutrient deficiencies.
People in this age group experience a wide variety of health conditions and physical abilities. To meet those needs, this guide includes information for a wide range of circumstances.
This information offers general guidance. For personal advice, talk with your primary care provider. Some people may also consult specialists such as registered dietitian nutritionists, physical therapists and occupational therapists.
Key nutrients for older adults
Calories
Calories from fat, protein and carbohydrates provide the energy older adults need to maintain basic bodily functions and be active. As adults get older, energy needs usually decrease. This is attributed mostly to a decline in physical activity and changes in metabolism.
Some changes that come with age may make it harder to get enough calories to support energy needs. These include changes in mobility, difficulty with chewing and swallowing, and general loss of appetite.
Not getting enough calories can lead to malnutrition, nutrient deficiencies and frailty.
Although calorie needs may decrease with aging, the body’s needs for some nutrients increase or stay the same. This can make it challenging for older adults to get all the nutrients needed without consuming too many calories.
Protein
Getting enough protein can be challenging for older adults.
Some people can't afford the high cost of meat and seafood. Others suffer dental or oral health issues that make it hard to chew or swallow. Some people experience a decreased appetite.
People who don't get enough protein can suffer from edema or decreased muscle mass. Other effects include dull skin and dry or brittle hair.
Another concern for older adults is sarcopenia, which is the loss of muscle mass. This condition can impair activities of daily living and increase the risk of falls. It is important for older adults to consume enough protein to maintain muscle.
Foods high in protein are meat, poultry, fish, shellfish, eggs, milk, cheese and yogurt. Protein is also found in grains, nuts, seeds and legumes such as beans, peas and lentils. To find out how much protein is in these foods, look at the nutrition facts labels on food packaging. Adults need 0.8 grams of protein for every 1 kilogram of body weight, or 0.36 grams for every 1 pound of body weight.
Older adults may need more protein than other adults because of changes due to aging, recovery from surgery and wound healing. Research suggests that older adults who eat protein with every meal have lower risks for protein deficiency and sarcopenia. For those reasons, older adults should try to eat 20–30 grams of protein at every meal. Table 1 includes examples of meals that have 20 grams of protein.
Fiber
Fiber is a type of carbohydrate. But unlike other carbohydrates, it cannot be digested. Fiber helps:
- Move food through the digestive system.
- Reduce constipation
- Improve blood glucose control
- Improve blood cholesterol levels.
Men older than 50 need 28 grams per day. Women older than 50 need 22 grams per day. Foods high in fiber include fruits, vegetables, nuts, whole grains and legumes such as beans, peas and lentils. Older adults who are not accustomed to consuming fiber should increase the amount slowly over time. Sudden increases in fiber intake can lead to gas, diarrhea and discomfort.
Vitamin D and calcium
Vitamin D and calcium are important nutrients for older adults because of their roles in supporting bone health. People who don't get enough vitamin D and calcium can suffer from osteopenia and osteoporosis. These disorders weaken bones and increase the risk of fractures. Older adults can struggle to get enough calcium from food alone, so taking supplements may be useful for some people.
Dairy foods including milk, yogurt and cheese are the best sources of calcium. Other calcium-rich foods are broccoli, bok choy, collard greens, kale and calcium-processed tofu. Some beverages are fortified with calcium, such as fruit juices and plant-based beverages like almond milk and soy milk.
Our bodies are able to make vitamin D when our skin is exposed to sunlight. In the Pacific Northwest, older adults may not make enough from sun exposure alone. Older adults may need to get vitamin D from food and supplements.
Vitamin D occurs naturally in only a few foods such as egg yolks and fatty fish like tuna, salmon, mackerel. It is also found in fortified foods like milk, breakfast cereals and juices.
Getting too much calcium and vitamin D from supplements is harmful, so it is important not to exceed the amounts needed. Obtain these nutrients from food rather than supplements, if possible. If using supplements, take no more than 2,000 mg of calcium per day and 100 micrograms of vitamin D per day.
Older adults taking supplements should speak with a health care provider or registered dietitian nutritionist. The provider can talk about the dose amount and interactions with other medications.
Vitamin B-12
Research estimates that up to 15% of older adults are deficient in vitamin B-12 and another 20% are at risk for deficiency. B-12 deficiency leads to macrocytic anemia and neurologic complications. Symptoms include fatigue, pale skin, loss of appetite, tingling and numbness in the limbs, gait disturbances, difficulty concentrating, memory loss, disorientation and dementia. Research also indicates that B-12 deficiency may contribute to depression, dementia and cardiovascular disease.
Many older adults lose the ability to absorb B-12, a condition called pernicious anemia. Pernicious anemia can also be caused by atrophic gastritis. This condition involves a weakening of the stomach lining and a drop in acid production, which is required for B-12 absorption.
B-12 occurs naturally in foods that come from animals, including meat, poultry, fish, shellfish, eggs, milk, cheese and yogurt. B-12 can also be found in some nutritional yeasts and fortified breakfast cereals. The amount of B-12 that can be absorbed from food during one meal is limited, so try to eat foods rich in B-12 at every meal.
People who do not consume foods that come from animals should consult a health provider. A registered dietitian nutritionist can provide information about supplements and other treatments.
Antioxidants
During normal cellular processes, compounds called free radicals can cause damage to DNA, cells and tissues. Antioxidants are substances that neutralize free radicals in our bodies to prevent them from doing harm. Research links antioxidants to protection against cancer, heart disease and other chronic illnesses.
Vitamin C, vitamin E, copper, zinc, selenium and manganese are examples of antioxidant nutrients. Other plant-based compounds called phytochemicals act as antioxidants. These include carotenoids (beta-carotene, zeaxanthin, and lutein) and flavonoids.
Some studies have shown that antioxidant nutrients and carotenoids may help reduce the risk for or delay the progression of cataracts and age-related macular degeneration. But there is not enough evidence for supplements. Taking too much of these substances in supplements can have serious negative effects.
Deficiencies in antioxidant vitamins (vitamins C and E) and minerals (copper, zinc, selenium and manganese) can lead to cognitive impairment and potentially worsen conditions like Alzheimer’s disease.
Fruits and vegetables that are red, orange, yellow and purple tend to be high in antioxidant phytochemicals and vitamin C. Good sources of vitamin E are whole grains, nuts, fruits and meats. Antioxidant minerals are found in meat, seafood, whole grains, fruits and vegetables.
Consuming 3–5 cups of fruits and vegetables every day will provide older adults enough antioxidant nutrients and phytochemicals. Taking additional supplements is of limited benefit, research shows.
Water
Dehydration can be an issue for older adults, especially those 85 or older. Causes include:
- Decreases in thirst sensation.
- Changes in kidney function.
- Alterations in hormone function.
- Side effects from medications.
- Prior stroke.
- Uncontrolled diabetes.
Sometimes older adults do not drink enough water because they fear arthritis pain or incontinence.
The effects of dehydration can range in severity from constipation or fecal impaction to impaired mental function, inability to maintain blood pressure and death.
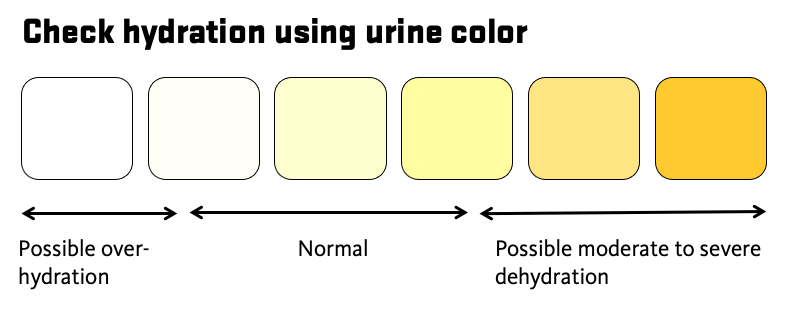
Water needs vary greatly from person to person, so there is no specific recommendation for the amount of water to drink each day. One of the best indicators of hydration is urine color — it should be light yellow to golden in color (Figure 1). If the color is dark yellow, drink more water. Urine may appear more yellow with certain medications or when taking multivitamins.
In addition to drinking water, people can get water from other beverages and food. Choose beverages low in added sugars and low in sodium. Nutrient-rich beverages like smoothies and milk also contain water. It was once thought that people should avoid coffee and tea because of the diuretic effects of caffeine. But recent research suggests consuming these beverages in moderation supports hydration. Foods that are good sources of water include fresh fruits and vegetables, as well as soups and stews.
Changes in physical health and everyday life that affect nutrition status
With aging come physiological changes in body systems. A loss of muscle mass and reduced energy needs may contribute to changes in dietary needs, physical functioning and mobility. There are several strategies older adults can use to reduce the risk of malnutrition.
Difficulty chewing and swallowing
Oral conditions common in older adulthood — such as tooth loss, gum disease, ill-fitting dentures and pain from tooth decay — can create issues with chewing. Some conditions can affect the ability to swallow. These include dehydration, certain medications and loss of muscle control due to Parkinson’s disease or dementia.
Issues with chewing and swallowing can lead people to avoid certain foods. This causes a monotonous diet and malnutrition. People commonly avoid meat and vegetables due to difficulty chewing. This can lead to numerous nutrient deficiencies.
Those who experience difficulty chewing and swallowing can choose soft protein foods like yogurt; soft-cooked or scrambled eggs; soup; smoothies; and meats that are ground, stewed and braised.
For easier swallowing, add moisture and fats such as gravy, salad dressing, olive oil and avocado. Prepare foods high in moisture like smoothies, soups and stews.
Diminishing taste and smell
Changes in smell and taste can influence the type and amount of food eaten by older adults. This diminished sense of smell and taste has been associated with a reduced interest in eating and less variation in foods. Some medications can also affect the sense of taste. This can lead to a decreased desire to eat and risk of nutrient deficiency.
Herbs and spices can boost the flavors and aromas of food. Add oregano, mint, sage, basil, rosemary, chili powder, coriander, cumin or cinnamon to enhance the eating experience. Lemon juice or other citrus can also brighten flavors. If you are limiting your sodium intake, choose herb and spice blends that do not contain salt or sodium.
Changes in mobility
Some people experience changes in physical mobility due to cognitive changes, injury, arthritis, and the loss of vision and hearing, among other conditions. This can put older adults at risk for nutrient deficiency. They could have difficulty shopping, preparing food, cooking and eating.
Arthritis pain and other mobility limitations can make it hard to prepare food. These strategies can help:
- Use pre-cut frozen or canned vegetables.
- Prepare foods while sitting at a table.
- To fill pots for boiling, set the pot on the stove and use smaller containers to fill it.
- Use an electric can opener.
If tremors make it challenging to eat, try weighted utensils and cups to increase stability. Occupational therapists can help identify useful tools and other potential solutions.
Social isolation
Changes in mobility, limited income and other factors can lead to isolation. Isolation can increase risks for malnutrition and other health issues.
Eat with friends, neighbors or family members to stay socially engaged and support your nutritional health. Contact area agencies on aging or places of worship about home visits and congregate or delivered meals. If visiting in person is not possible, enjoy a meal with someone while talking on the phone or a video call.
Changes in digestion
Some health conditions and medications can affect digestion, including constipation, increased gas, bloating and loss of muscle control that slows the movement of food through the digestive system.
Increasing physical activity is key to a healthy gastrointestinal system. Being more active can improve function and ease symptoms. Changing your food intake to lessen symptoms can lead to nutrient deficiency. Older adults who are experiencing problems with gastrointestinal function should consult with a primary care physician or registered dietitian nutritionist to discuss strategies that can help.
Nutrition and chronic disease
Another major health concern for older adults is chronic disease, including heart disease, cancer and diabetes. Research shows that following healthy eating patterns that focus on increasing fruits and vegetables, eating lean proteins, consuming dairy and eating whole grains can reduce the risk of chronic diseases.
MyPlate.gov is a resource with information about how to follow healthy eating patterns to reduce the risk for chronic disease. Older adults with chronic disease may need additional changes to support their health, so it is important to speak with a primary care physician or registered dietitian nutritionist.
Improving nutritional health with physical activity
Being physically active has numerous nutritional benefits for older adults. The extra calories burned during physical activity increase energy requirements. This can help stimulate appetite and increase food intake. Physical activity can also help improve digestion and symptoms of constipation.
Health experts recommend older adults be active for 150 minutes per week. Choose a mixture of aerobic, balance, flexibility and strength-building movement, such as Better Bones and Balance, StrongWomen and Walk with Ease.
Those beginning an exercise program should consult a physician and increase exercise gradually.
References
Ahmed, T., N. Haboub. (2010). Assessment and management of nutrition in older people and its importance to health. Clinical Interventions in Aging. 5:2017-216.
Institute of Medicine of the National Academies of Science. (2006). Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington D.C.: National Academies Press.
Leslie, W., C. Hankey. (2015). Aging, Nutritional Status and Health. Healthcare (Basel). 3(3): 648-658.
National Institute of Diabetes and Digestive and Kidney Diseases. Health Tips for Older Adults. Accessed Sept. 10, 2019,
National Institutes of Health Office of Dietary Supplements. Vitamin B12 Fact Sheet for Health Professionals. Washington D.C.: U.S. Department of Health & Human Services. Accessed Sept.10, 2019.
National Institutes of Health Office of Dietary Supplements. Vitamin D Fact Sheet for Health. Accessed Oct. 8, 2019.
National Institutes of Health National Center for Complementary and Integrative Health. Probiotics. Accessed Oct. 8, 2019.
Position of the Academy of Nutrition and Dietetics Food and Nutrition for Older Adults: Promoting Health and Wellness. (2012). Journal of the Academy of Nutrition and Dietetics. 112(8): 1255-1277.
Position of the Academy of Nutrition and Dietetics; Micronutrient Supplementation. (2018). Journal of the Academy of Nutrition and Dietetics. 118(11):2162-2173.
Traylor, D.A., S.H.M. Gorrissen, S.M. Phillips. (2018). Perspective: Protein Requirements and Optimal Intakes in Aging: Are We Ready to Recommend More than the Recommended Daily Allowance? Advances in Nutrition. 9:171-182.
U.S. Department of Health and Human Services and U.S. Department of Agriculture. (2015). 2020-2025 Dietary Guidelines for Americans. Ninth Edition. December 2020. Accessed March 9, 2021.
U.S. Department of Health and Human Services. (2019). Physical Activity Guidelines for Americans. Second Edition. Washington D.C. Accessed Sept. 11, 2019.